ICD-10 CM (Diagnosis) and PCS (Procedure) Codes
The International Classification of Diseases, Tenth Edition (ICD-10) is a clinical cataloging system that went into effect for the U.S. healthcare industry on Oct. 1, 2015, after a series of lengthy delays. Accounting for modern advances in clinical treatment and medical devices, ICD-10 codes offer many more classification options compared to those found in predecessor ICD-9.
ICD-10 Clinical Modification (ICD-10-CM) is a system used by physicians and other healthcare providers to classify and code all diagnoses, symptoms and procedures recorded in conjunction with hospital care in the United States. ICD-10-CM codes provide the ability to track and reveal more information about the quality of healthcare, allowing healthcare providers to better understand medical complications, better design treatment and care, and better comprehend and determine the outcome of care.
ICD-10 Procedure Coding System (ICD-10-PCS) is a system of medical classification used for procedural codes that track various health interventions taken by medical professionals. ICD-10-PCS is a completely separate medical coding system from ICD-10-CM, containing an additional 87,000 codes for use ONLY in United States inpatient, hospital settings. Common procedures, lab tests, and educational sessions that are not unique to the inpatient, hospital setting have been omitted from ICD-10-PCS. ICD-10-PCS codes must be used on all HIPAA transactions, starting in October 2013.
ICD-10 CM (Diagnosis)
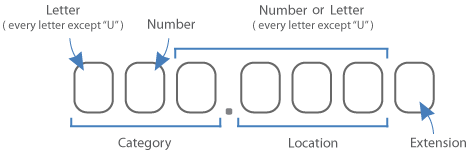
ICD-10-CM is a seven-character, alphanumeric code. Each code begins with an alphabetic letter. That letter is followed by two numbers. The first three characters of ICD-10-CM are the “category.” The category describes the general type of the injury or disease. The category is followed by a decimal point and the subcategory. This is followed by up to two subclassifications, which further explain the cause, manifestation, location, severity, and type of injury or disease. The last character is the extension. Alphabetic digits are not case sensitive. Decimal is after third digit.
ICD-10 PCS (Procedure)
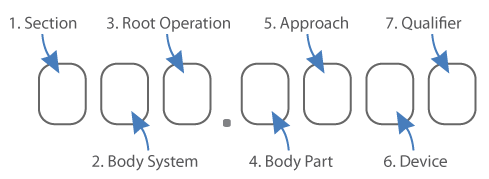
The system uses three to seven digit alphanumeric codes to specify medical procedures. Each character can be any of 34 possible values the ten digits 0-9 and the 24 letters; the letters “O” and “I” are excluded to avoid confusion with the numbers “0” and “1”. The first digit indicates the section of medical practice (surgery, administration, measuring and monitoring, etc.) and the following digits specify the body system , root operation, body part, approach and the device used. The seventh character is a qualifying digit. No decimal is used.
GEM (General Equivalence Mapping) 2018
General Equivalence Mapping (GEM) refers to the mapping tools designed and used to perform an ICD-9 to ICD-10 crosswalk.
The conversion will not always result in simple one-to-one mapping. While some ICD-9 codes do map directly to an ICD-10 code, it does not always mean the codes match in detail. Many codes will require additional information in order to correctly map the intended ICD-10 code; information such as, cause, location, type of encounter, etc. Some ICD-diagnosis codes, like those pregnancy and obstetrics, will garner a one-to-three crosswalk, depending on the stage and complication of pregnancy. In extreme cases, like the coding of fractures and disorders of the bone and cartilage, the ICD-9 to ICD-10 crosswalk can result in ICD-10 mapping that yields hundreds to thousands of results. For a period of two years or more, systems will need to access both ICD-9-CM codes and ICD-10-CM codes as the country transitions from ICD-9-CM to ICD-10-CM. Mapping will be necessary so that equivalent codes can be found for issues of disease tracking, medical necessity edits and outcomes studies.
Medicare Severity — Diagnosis Related Group (MS-DRG) v43.0
The Social Security Act created a system of payment for the operating costs associated with Medicare Part A hospital inpatient stays. This system is based on set rates and is referred to as the Inpatient Prospective Payment System (IPPS). As a part of this system, each case is categorized into a Medicare Severity — Diagnosis Related Group (MS-DRG).
Patients who have similar clinical characteristics and similar treatment costs are assigned to an MS-DRG. The MS-DRG is linked to a fixed payment amount based on the average treatment cost of patients in the group. Patients can be assigned to an MS-DRG based on their diagnosis, surgical procedures, age, and other information. Hospitals provide this information on their Medicare claim, and Medicare uses this information to decide how much the hospitals should be paid.